What Is Keratoconus?
Keratoconus is an eye condition affecting the clear front surface of the eye. Known as the cornea, this curved front surface acts like the windscreen of a car. Keratoconus is a progressive disease, resulting in distortion of the cornea, in turn affecting eye sight.
In keratoconus, the central cornea becomes thinner and thinner. As a result of this thinning, the cornea becomes weaker, and bulges, or buckles in this area. As the cone advances, the distortion increases, further reducing vision.
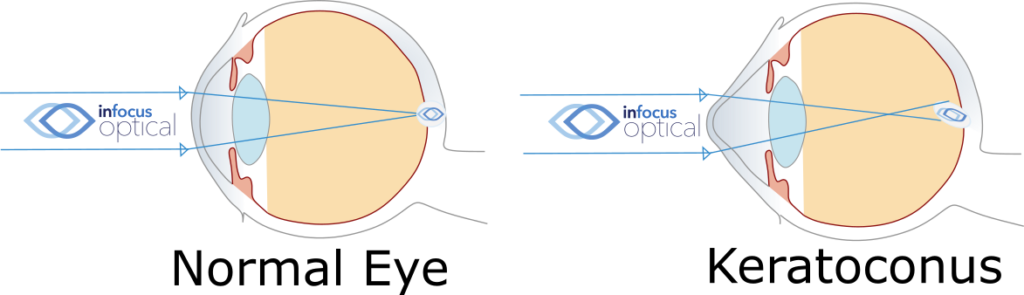
The normal cornea has an evenly rounded front surface, much like a basketball or soccer ball. The thinned cornea bulges into a cone shape. The word keratoconus has Greek and Latin roots, translating to ‘cone-like cornea’. So, instead of being shaped like a round ball, the cornea is more like the tip of a rugby or AFL football.

As a consequence of the irregular cornea, keratoconus results in a decreasing quality of vision. This is often most noticeable at night time with car head lights or street lamps. Specifically, keratoconus often causes haloes and ghosting around lights. This is because the cone shaped cornea focuses light into many different points instead of a crisp and clear image.
While keratoconus usually affects both eyes, sometimes the severity can differ between the eyes a lot. For this reason, some one eye advanced cases receive a late diagnosis. This can be because the patient is still seeing very well from the better eye. With this in mind, it is always best to have eye tests regularly for all sorts of eye conditions.
Why Do I Have Keratoconus?
We believe keratoconus affects 1 in 1500 people. In particular the causes are not fully known. Indeed, we think there are genetic and environmental factors. In fact, it is not uncommon to have no known family history.
Indeed, the most common association is eye rubbing. That is to say, we will commonly note a history of significant eye rubbing with keratoconus. Usually eye rubbing may be due to hay fever, allergies, eczema or other triggers. In keratoconus, eye rubbing breaks down the tissue fibers of the cornea. This mechanical rearrangement of fibers causes weakening of the cornea. However, on top of this physical damage, eye rubbing causes release of enzymes in the cornea. The enzymes further degrade the corneal bonds. This leads to further weakening and subsequent thinning.
Will I Go Blind From Keratoconus?
In severe keratoconus, vision can approach legal blindness. However, it is very unlikely to go totally blind. Especially with the treatments on-hand today. While vision quality worsens with severity, it can be restored to some extent. This may be with contact lenses or surgery.
Most importantly, if detected early, further deterioration can be prevented. This can simply be from managing eye rubbing for some. For others, the cross-linking procedure may be advised. Advanced cases can cause scarring of the cornea. Scarring can result in further vision loss. For this reason, book an eye test with our optometrists at InFocus Optical today.
How Is Keratoconus Treated?
In the early stages, the condition can be difficult to detect. Glasses can correct vision in mild cones. At this stage, soft contact lenses can also be a good option. But what often happens is a frequently changing prescription. Especially a variable amount and degree of astigmatism. These changes can often be the first signs.
Hard Contact Lenses
In moderate cases, glasses and soft contacts cannot fully correct vision. This is when hard contact lenses become the main form of treatment. Also known as rigid gas permeable, or RGPs, these lenses are custom made for each eye. These specialty contact lenses are designed to closely match the shape of your eye. The round front surface is the ideal shape to focus light thus allows good vision. Being a hard lens, the shape is fixed, unlike a soft lens. So, instead of a pointy cone front surface, we regain a smooth eye surface.
Further advanced designs include piggy back, hybrid and miniscleral contact lenses. Our optometrist at InFocus Optical will discuss the best option to suit your needs. Regardless of the lens type, all contact lenses for keratoconus are custom designed. Our labs then manufacture lenses to the individual eye.
Corneal Graft
In severe cases of keratoconus, the cornea may become scarred. If corneal scarring is so bad that contact lenses do not help, we may need a corneal graft. Also called corneal transplanting, it involves replacing the scarred cornea tissue. After a graft, it may take up to two years for the healing process. Many cases may still be require a rigid contact lens after a graft. For these reasons, grafting is only after all other options fail to help. Generally, good keratoconus management prevents the need for a graft.
Corneal Collagen Cross-Linking
In order to prevent progression, corneal collagen cross-linking (CXL) is the main procedure for the worsening eye. Research shows cross-linking slows down, and even stops, the progression. By closely monitoring the corneal shape, our optometrists at InFocus Optical will advise when referral to an eye surgeon is necessary. We work closely with many corneal specialists to ensure your eye condition is well managed. If you need an eye specialist, come see our optometrist.
How Do You Diagnose Keratoconus?
The early stages of keratoconus can often be hard to detect. For some, the first eye test is often when keratoconus is severe! Signs and symptoms may include eye rubbing and blurry vision. You may notice haloes, ghosting, distortion or double vision. Parents of a child with keratoconus should be aware of a constantly changing prescription.
Our optometrist will check your:
- vision
- prescription
- corneal thickness
- corneal curvature
Specifically, we are looking for reduced vision. The cause being irregular astigmatism on the eye. This would be the result of thinned and steep corneas. Further signs might include a scissors reflex in retinoscopy. Our microscope allows detection of corneal steepening or scarring. We may also see corneal nerves or Vogt’s striae among other signs. Ultimately, our corneal topographer will show an eye shape indicative of a cone.
Accordingly, the we monitor these measurements to detect worsening. Book an eye test with our optometrist today.
Keratoconus Australia is a non-profit support network for this eye condition. They offer further resources and information for patients and carers.
